Iboga, which contains Ibogaine, can be an effective treatment for addiction that also comes with some potential risks. So practicing harm reduction is a vital component of receiving the healing benefits of this therapy. Join Ryan Rich, Lead Iboga Provider at Root Healing, as we explore recommended harm reduction practices for Iboga and Ibogaine.
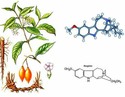
Ibogaine is an alkaloid naturally found in the Tabernanthe Iboga shrub. The inner root bark of this shrub, called Iboga, has been used for thousands of years in the West-African Bwiti tradition. The Bwiti use Iboga in rituals for physical healing, spiritual healing, and spiritual discovery. However, in modern times, both forms are used outside of the Bwiti context for their many healing benefits. The most popular being the treatment of addiction, as Iboga is particularly effective for opioid addiction [1]. Therefore, the scientific world is just now catching up with Iboga’s promising healing potential in the treatment of Parkinson’s, PTSD, and trauma, to name a few.
As a result of all this exciting new information and the often high cost of treatment, some may feel compelled to try to take Iboga, Ibogaine, or Iboga TA (total alkaloid extract) on their own. We DO NOT recommend this. Thus, it is our recommendation to always work with an experienced team for everything from microdosing Iboga to a full-on Ibogaine Detox.
Iboga, Ibogaine, and Harm Reduction
So in the context of Iboga and Ibogaine harm reduction, we worked with our own medical team at Root Healing to write this article. So, the purpose of this article is to go over the physical contraindications, drug interactions, and proper preparation for a safe, therapeutic experience with Ibogaine. Keep in mind that following the strategies for harm reduction does not dismiss the need for medical supervision during the treatment. Therefore, make sure to always work with an experienced team including physicians and Bwiti-trained experts.
Iboga, when taken with an experienced team and proper screening, is very safe. Many retreat centers, like ours, work with Iboga in the traditional Bwiti way, but also work with a medical team ensuring proper screening and safe ceremonies. The screening process is one of the most important aspects of our work.
Ibogaine, the chemical extract of Iboga, is more dangerous and requires stricter medical protocols. Consequently, most of the reported incidents and fatalities were with Ibogaine (not Iboga) and could have been prevented with a qualified team.
Above all, using Iboga or Ibogaine without proper preparation and supervision is dangerous and must be avoided. So at the very least, please consider these things:
Physical Risks and Contraindications for Iboga and Ibogaine
Heart Conditions
The main organ that can be negatively affected by ibogaine therapy is the heart. That’s because ibogaine’s metabolite, called noribogaine, blocks some of the ion channels in the cardiac muscle, which regulate the normal rhythm [2].
More specifically, those are the potassium ion channels called Kv11.1. They are commonly inhibited as a side-effect by many prescription medications, including antiarrhythmics, anti-psychotics, and certain antibiotics.
So this results in slower repolarization of the heart and increased risk for a life-threatening arrhythmia called Torsades de pointes [2]. The blockage of the potassium channel is never permanent. The duration of the effect depends on the half-life of the medication, which in the case of Ibogaine is 28-49 h [3].
Slower repolarization can be detected as a prolonged QT-interval via a regular electrocardiogram (ECG). Thus, an ECG performed by a medical doctor is one of the mandatory tests before an Iboga treatment.
Reasons for a long QT interval may include medications, inherited genetic conditions, malnourishment, loss of electrolytes, and chronic cardiovascular diseases such as heart failure. If you have any heart disease or another contraindication that may prolong the QT interval, then this therapy may be contraindicated. Factors which prolong the QT interval are concerning, as Ibogaine will further slow down the repolarization leading to potentially fatal consequences.
To sum up, there are few fatalities related to Iboga use. According to the medical records, all of the patients have been chronically ill or took contraindicated medications [4].
We strongly recommend getting an ECG/EKG and sharing the results with your doctor or an experienced team prior to taking Ibogaine.
Liver Conditions
The negative effects on the heart can be increased if Ibogaine is not effectively neutralized by the liver. This can occur due to hepatitis, cirrhosis, or another condition that impedes liver function.
Normal hepatic function is imperative for safe ibogaine therapy because the liver enzymes, called CYP450 2D6, have the main role in neutralizing the alkaloid [5].
Diseases or medications which hinder the function of the enzymes can lead to increased bioavailability of Ibogaine. This results in prolonged exposure and elevated serum concentrations of the alkaloid. This increases the risk for severe side effects and arrhythmia.
People with chronic liver diseases are at a particularly increased risk. Likewise, there are reports of fatalities after ibogaine use in patients with liver cirrhosis [6].
Thus, liver function tests are another mandatory element of the preparation for ibogaine treatment. Your hepatic panel includes information for liver enzyme levels, serum proteins, coagulation, and other useful biomarkers of liver injury.
Taking care of your liver health is crucial before a treatment. You must abstain from drinking alcohol for at least a week before your Iboga therapy. If you are a chronic drinker or addicted to alcohol, please consult with your doctor prior to any retreat on how best to detox.
Drug Interactions
The QT interval and CYP450 2D6 enzyme are commonly affected by many prescription medications. If you are taking a drug that affects either or both of them, it must be tapered off before Ibogaine treatment. Otherwise, it will significantly increase the risk for adverse reactions.
For example, antidepressants such as selective serotonin reuptake inhibitors (SSRIs) block the 2D6 enzyme and prolong the QT-interval, which makes combinations with ibogaine extremely dangerous [7].
Similarly, other medications which block CYP450 2D6 and prolong the QT-interval include [8]:
- Antidepressants (not only SSRIs)
- Antiarrhythmics
- Antifungal
- Antihistamines
- Quinine (Antimalarial)
- Antipsychotics
- Some antibiotics
So patients with an addiction to opioids or stimulants require a specific tailored treatment that takes into consideration these drugs and their effect on the liver. Narcotics and medications which mainly affect the liver metabolism by blocking the 2D6 enzymes are [9]:
- Anti-HIV
- Cannabidiol (CBD)
- Antacids
- Opioids and methadone
- Cocaine and stimulants
- Beta-blockers
- Antiemetics
In addition, benzodiazepines and other medications that depress the nervous system must be safely tapered off prior to any treatment. Talk to your doctor before discontinuing any medications. Some drugs have a rebound effect, which means your symptoms might get exacerbated and dangerous if you stop taking them abruptly. Your physician will provide you with information on how to taper off them properly.
To sum up, keep in mind that these lists are not exhaustive and any medication you are taking might have unknown contraindications. Thus, make sure to consult with a medical professional or experienced team beforehand and report all medications you have taken recently.
Dietary Recommendations for Iboga and Ibogaine Treatment
Fasting is strictly prohibited before ibogaine treatment. Patients who are fasting, or suffer from eating disorders such as bulimia and anorexia, are at an increased risk of prolonged QT due to electrolyte imbalances.
People who have recently had digestive symptoms such as vomiting or diarrhea are also at an increased risk.
Several foods and drinks can block the CYP450 2D6 enzyme and slow down the liver metabolism of ibogaine breakdown, leading to elevated concentrations and side effects [10]. Those are grapefruit, pomelo, and their juices.
Quinine-containing drinks such as tonic water and bitter lemon are also contraindicated. They must be avoided in the days before ibogaine treatment to minimize the risks for side effects [11].
Summary of Physical Contraindications for Iboga and Ibogaine
In short, the main physical contraindications against ibogaine treatment include factors that might slow down the repolarization of the heart and block the detoxification systems of the liver. These factors are:
- Cardiovascular conditions
- Liver conditions
- Drugs and medications
- Certain foods and beverages (including alcohol)
In conclusion, while Iboga and Ibogaine can be a safe and effective treatment, for the reasons outlined above, we do not recommend doing it without an experienced team.
References
- Davis AK, Barsuglia JP, Windham-Herman AM, Lynch M, Polanco M. Subjective effectiveness of ibogaine treatment for problematic opioid consumption: Short- and long-term outcomes and current psychological functioning. J Psychedelic Stud. 2017 Nov;1(2):65-73. doi: 10.1556/2054.01.2017.009. Epub 2017 Oct 17. PMID: 30272050; PMCID: PMC6157925.
- Koenig, X., Kovar, M., Boehm, S., Sandtner, W., & Hilber, K. (2014). Anti-addiction drug ibogaine inhibits hERG channels: a cardiac arrhythmia risk. Addiction biology, 19(2), 237–239. https://doi.org/10.1111/j.1369-1600.2012.00447.x
- Sanguinetti, M. C., & Tristani-Firouzi, M. (2006). hERG potassium channels and cardiac arrhythmia. Nature, 440(7083), 463–469. https://doi.org/10.1038/nature04710
- Glue, P., Lockhart, M., Lam, F., Hung, N., Hung, C. T., & Friedhoff, L. (2015). Ascending-dose study of noribogaine in healthy volunteers: pharmacokinetics, pharmacodynamics, safety, and tolerability. Journal of clinical pharmacology, 55(2), 189–194. https://doi.org/10.1002/jcph.404
- Alper, K. R., Stajić, M., & Gill, J. R. (2012). Fatalities temporally associated with the ingestion of ibogaine. Journal of forensic sciences, 57(2), 398–412. https://doi.org/10.1111/j.1556-4029.2011.02008.x
- Obach, R. S., Pablo, J., & Mash, D. C. (1998). Cytochrome P4502D6 catalyzes the O-demethylation of the psychoactive alkaloid ibogaine to 12-hydroxyibogamine. Drug metabolism and disposition: the biological fate of chemicals, 26(8), 764–768.
- Papadodima, S. A., Dona, A., Evaggelakos, C. I., Goutas, N., & Athanaselis, S. A. (2013). Ibogaine related sudden death: a case report. Journal of forensic and legal medicine, 20(7), 809–811. https://doi.org/10.1016/j.jflm.2013.06.032
- Ereshefsky, L., Riesenman, C., & Lam, Y. W. (1995). Antidepressant drug interactions and the cytochrome P450 system. The role of cytochrome P450 2D6. Clinical pharmacokinetics, 29 Suppl 1, 10–19. https://doi.org/10.2165/00003088-199500291-00004
- Nachimuthu, S., Assar, M. D., & Schussler, J. M. (2012). Drug-induced QT interval prolongation: mechanisms and clinical management. Therapeutic advances in drug safety, 3(5), 241–253. https://doi.org/10.1177/2042098612454283
- de la Torre, R., Yubero-Lahoz, S., Pardo-Lozano, R., & Farré, M. (2012). MDMA, methamphetamine, and CYP2D6 pharmacogenetics: what is clinically relevant?. Frontiers in genetics, 3, 235. https://doi.org/10.3389/fgene.2012.00235
- Girennavar, B., Poulose, S. M., Jayaprakasha, G. K., Bhat, N. G., & Patil, B. S. (2006). Furocoumarins from grapefruit juice and their effect on human CYP 3A4 and CYP 1B1 isoenzymes. Bioorganic & medicinal chemistry, 14(8), 2606–2612. https://doi.org/10.1016/j.bmc.2005.11.039