Journal of Psychopharmacology reports enduring benefits after MDMA for post-traumatic stress disorder symptom improvement lasting years after treatment. After participating in clinical trials of MDMA-assisted psychotherapy, people who had suffered from chronic PTSD experienced significant symptom reduction. This includes better relationships, increased appreciation for life, and a greater sense of possibility and spirituality. Principal Investigator Dr. Michael Mithoefer talks about the treatment approach and factors influencing the treatment response.
Results of Six Phase 2 Clinical Trials
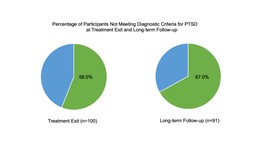
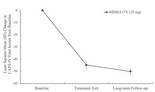
The journal Psychopharmacology [1] published long-term participant outcomes in six phase 2 clinical trials investigating MDMA-assisted psychotherapy for PTSD. The treatment approach includes 2-3 psychotherapy sessions with MDMA, bookended by preparatory and integrative sessions. Two months following the last session, PTSD symptoms saw a significant reduction. 56% of participants no longer met PTSD criteria. 91 participants conducted follow-ups twelve months later, or on average of 3.8 years in one study. Follow-ups reassess symptoms and quality of life. Of these, 67% did not meet PTSD criteria at the long-term follow-up. Furthermore, many reported substantial improvements in various life aspects, including relationships, sleep quality, and general wellbeing.
MDMA-assisted psychotherapy involves around 40 hours of therapy with a male/female co-therapy team. The MDMA sessions last for 6-8 hours. Secondly, other non-drug 90-minute sessions are used for preparation and integration.
Dr. Michael Mithoefor, a psychiatrist served as the principal investigator and lead therapist on two of the trials. He commented on what psychological factors he thought influenced the response to treatment.
“One of the most intriguing factors is that many people who have PTSD and have tried various types of treatment without success, very early in their MDMA experience, arrive at an ‘inner knowing’ that they are going to be able to heal. It’s striking that when this happens it’s far from the end of the story. They still need to do a lot of trauma processing that is usually very painful even with MDMA, but somehow they suddenly know they are going to be able to do this.”
Easier Navigation of Difficult Emotions
MDMA-assisted psychotherapy shares many key tenets of traditional therapies. However, it’s the drug’s effects that enable a person to more readily navigate difficult emotions when recalling traumatic memories. Dr. Mithoefer describes the phenomenon.
“This may relate to changes in patterns of connectivity in the brain that are observed in imaging studies of MDMA, that can allow for new perspectives and different responses from entrenched patterns resulting from old trauma.”
Brain imaging studies have visualized the amygdala. The amygdala is a region in the brain known to be activated during a fear response, and to be quieted after MDMA administration [2,3]. This may be one of the reasons why people with PTSD can easily face and process traumatic memories during MDMA sessions. Dr. Mithoefer continues the analysis.
“Other psychological factors have to do with a sense of decreased defensiveness about revisiting painful experiences, a sense of greater connection to other people and greater acceptance of self and others.”
“I think that the MDMA gave me the ability to feel as though I was capable and safe of tackling the issues. I felt like I had the ability and tools. Whereas before I was unarmed, unarmored, and had no support. And this type of environment, with (the therapists), the catalyst drug, and everything else, it felt as though I had backup. Now it was safe and I had my tools and weapons to be able to tackle the obstacles that I never had before” Study Participant [4].
The published results showed scores on the Clinician Administered PTSD Scale (CAPS-4) dropped from baseline to the end of treatment (-44.8). Similarly, they continued to decline at the long-term follow-up (-5.2).
MDMA-Assisted Psychotherapy for PTSD= Growth
In addition to basic symptom improvement, other measures in these studies looked at post-traumatic growth. Post-traumatic growth refers to specific changes in self-perception, interpersonal relationships, or philosophy of life. The more PTSD symptoms improved, the more growth in these areas did too [5]. Overall, after undergoing MDMA-assisted psychotherapy participants reported having better relationships, increased appreciation for life, and a greater sense of possibility and spirituality. After that, the response was enduring for many at the long-term follow-up.
“I’ve done some really weird and amazing stuff since I’ve come out of this study. I had this drive before, but I had this thing holding me back. And it’s like the gates were opened and I just…ran. So I do end up butting up against triggers and stuff like that occasionally. But it’s because I’m doing way more” Study Participant [4].
But as with most interventions, not everyone’s PTSD symptoms resolve after MDMA therapy. For instance, what factors influence treatment outcomes? Can we predict who is most likely to respond?
While these questions are actively being investigated, Dr. Mithoefer weighed in.
“Perhaps most important are a willingness to engage in a deep process and a commitment, and proper support to work to integrate the MDMA experiences . Unlike most psychiatric medicines, MDMA does not act by directly suppressing symptoms. It appears to work by catalyzing a psychotherapeutic process that can be challenging along the way and can be problematic without commitment and support to work through and integrate the challenges.”
People seeking this approach can’t simply rely on the MDMA experience to relieve their PTSD. However, they must fully engage in the therapeutic process and be dedicated and open to making positive changes in their lives.
MDMA-Assisted Psychotherapy for PTSD Breakthrough
The Food and Drug Administration (FDA) evaluated both the short- and long-term results from these studies [6]. Ultimately the FDA granted a Breakthrough Therapy designation for MDMA-assisted psychotherapy in 2017. After nearly 2 decades of conducting this research, Dr. Mithoefer conveyed enthusiasm.
“This is an exciting time in MDMA research. We are on the cusp of determining whether Phase 3 clinical studies will lead to FDA approval of MDMA as a medicine for legal clinical use. If that happens, not only will there be the opportunity to provide treatment for many people who need it, but research into a huge range of questions about other possible indications for treatment, mechanism of action, and the nature of psychological healing itself.”
Momentum continues in phase 3 trials. A recent interim analysis of 60 participants’ data in the first phase 3 trial showed at least a 90% probability of a statistical difference between the MDMA and placebo groups. Enrollment for these trials is ongoing. If both phase 3 trials show significant effects of MDMA-assisted psychotherapy, then this novel treatment approach could become a legal prescription medication for PTSD in 2022.
References
- Jerome, L., Feduccia, A.A., Wang, J.B., Hamilton, S., Yazar-Klosinski, B., Emerson, A., Mithoefer, M.C., & Doblin, R. (2020). Long-term follow-up outcomes of MDMA-assisted psychotherapy for treatment of PTSD: a longitudinal pooled analysis of six phase 2 trials. Psychopharmacology.
- Gamma, A., Buck, A., Berthold, T., Hell, D., & Vollenweider, F. X. (2000). 3, 4-Methylenedioxymethamphetamine (MDMA) modulates cortical and limbic brain activity as measured by [H215O]-PET in healthy humans. Neuropsychopharmacology, 23(4), 388-395.
- Carhart-Harris, R. L., Murphy, K., Leech, R., Erritzoe, D., Wall, M. B., Ferguson, B., … & Tanner, M. (2015). The effects of acutely administered 3, 4-methylenedioxymethamphetamine on spontaneous brain function in healthy volunteers measured with arterial spin labeling and blood oxygen level–dependent resting state functional connectivity. Biological psychiatry, 78(8), 554-562.
- Barone, W., Beck, J., Mitsunaga-Whitten, M., & Perl, P. (2019). Perceived benefits of MDMA-assisted psychotherapy beyond symptom reduction: qualitative follow-up study of a clinical trial for individuals with treatment-resistant PTSD. Journal of psychoactive drugs, 51(2), 199-208.
- Gorman, I., Belser, A. B., Jerome, L., Hennigan, C., Shechet, B., Hamilton, S., … & Feduccia, A. A. (2020). Posttraumatic Growth After MDMA‐Assisted Psychotherapy for Posttraumatic Stress Disorder. Journal of traumatic stress, 33(2), 161-170.
- Feduccia, A. A., Jerome, L., Klosinski, B., Emerson, A., Mithoefer, M. C., & Doblin, R. (2019). Breakthrough for Trauma Treatment: Safety and Efficacy of MDMA-Assisted Psychotherapy Compared to Paroxetine and Sertraline. Frontiers in psychiatry, 10, 650.