More discovery is needed around the response to MDMA-assisted psychotherapy. Many participants in phase 2 trials of MDMA-assisted psychotherapy for PTSD responded well to the treatment. But for some, PTSD symptoms are still present after MDMA and integration sessions. Can we predict who will respond? New evidence shows that prior use of a specific class of psychiatric medications reduces the effectiveness of MDMA-assisted psychotherapy. Read the full publication in the journal Psychopharmacology [1].
Six Phase 2 Trial Results
Results from six phase 2 trials of MDMA-assisted psychotherapy for PTSD indicated participants who were treated with MDMA had a greater reduction in symptom severity after two MDMA sessions than those who received a placebo control dose [2].
The FDA’s Breakthrough Therapy designation was based on safety outcomes and data showing more participants in the MDMA group (54.2%) did not meet criteria for PTSD compared to the control group (22.6%) following two experimental sessions [3]. Essentially, MDMA doubled the effect of psychotherapy alone. Moreover, it performed better than available PTSD medications (two antidepressant SSRIs).
On one hand, this is an extraordinary finding. On the other hand, we can’t help but wonder something else. What about the other 45.8% in the MDMA group that still had symptoms severe enough to maintain a diagnostic PTSD status? Are there any particular reasons why these participants’ symptoms failed to remit? To be sure, many of these individuals did show some signs of improvement. But not to the same degree as the high responders in the MDMA group.
Can we predict who will respond?
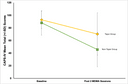
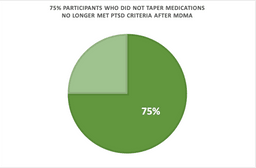
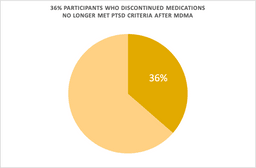
We wanted to understand if there were any factors to predict the treatment response. We found no relationship between PTSD symptom reduction and participant age, PTSD duration, sex, race, and prior self-reported “ecstasy” use [2]. However, in an exploratory analysis recently published in Psychopharmacology, we found that participants who tapered off specific types of psychiatric medications (reuptake inhibitors) had a blunted response to MDMA. Their blood pressure rose to a lesser degree during the MDMA sessions and their PTSD symptom severity didn’t change after MDMA-assisted psychotherapy as much as participants who did not taper off these medications [1].
MDMA changes a person’s subjective experience and elevates blood pressure, heart rate, and body temperature by increasing release of neurotransmitters. It does so by binding to and reversing transporter proteins that normally bring neurotransmitters back into the neuron.
Discontinuation of SSRIs
Medications classified as reuptake inhibitors are commonly prescribed for PTSD and depression. For example, think selective serotonin reuptake inhibitors (SSRIs). Several neural mechanisms produce the desired effects. After chronic use, there is a change in the number and function of the reuptake proteins the drugs target. As a result, this likely ties into how SSRIs work but also plays a role in the side effects people experience when they stop taking them [4].
So, upon discontinuing a reuptake inhibitor medication, a person may experience withdrawal symptoms as the brain adapts to no longer having the medication on board. These types of medications come with slow tapering recommendations. This allows neurotransmitter systems to adjust and minimize adverse symptoms, thus reducing the dose incrementally rather than stopping quickly. It’s unclear how long it takes for the serotonin system to reach equilibrium after discontinuation of reuptake inhibitors, some people experience withdrawal symptoms for weeks or even years [4].
Medications Affect Response to MDMA-assisted Psychotherapy
Participants in the MDMA trials were required to taper off psychiatric medications prior to the MDMA sessions, but even still these participants appear to have a different physiological response to MDMA and consequently, less of a reduction in PTSD and depression symptoms. Supportive of neurochemical mechanism, longer periods of abstinence prior to the MDMA sessions were associated with greater increases in body temperature when MDMA was administered.
This information is important for patients who may have only one shot at MDMA therapy. If longer periods of abstinence from specific psychiatric medications are possible, these findings suggest a person will have a better chance at seeing marked improvement in their PTSD symptoms. However, for some individuals, being off psychiatric medications can be too risky to their mental health and the possible benefits may not outweigh the risk of stopping medications.
Response to MDMA-assisted Psychotherapy Needs More Data
While these findings are intriguing and relevant for clinical applications, more data is needed from a larger sample. From phase 3 trials, we’ll have more detailed information about the length of tapers, how long people were on these medications prior to tapering, and variability in the abstinence period to further quantify the effects of medications on the MDMA experience. With the current body of evidence, we can’t rule out that the participants in the taper group weren’t by chance just harder to treat or had other factors precluding response to MDMA beyond tapering medications.
By understanding factors that affect treatment responses, we can potentially tailor the approach for any given individual. This is critically important for psychedelic-assisted therapies which have a limited number of administrations and are time intensive for both the patient and therapy team. From these exploratory analyses, we now have a guidepost on factors to adjust that will hopefully optimize the intervention to improve outcomes and reduce the cost of care.
References
- Feduccia, A. A., Jerome, L., A., Mithoefer, M. C., & Holland, J. (2020). Discontinuation of medications classified as reuptake inhibitors affects treatment response of MDMA-assisted psychotherapy. Psychopharmacology. https://link.springer.com/article/10.1007/s00213-020-05710-w
- Mithoefer, M. C., Feduccia, A. A., Jerome, L., Mithoefer, A., Wagner, M., Walsh, Z., … & Doblin, R. (2019). MDMA-assisted psychotherapy for treatment of PTSD: study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials. Psychopharmacology, 236(9), 2735-2745.
- Feduccia, A. A., Jerome, L., Klosinski, B., Emerson, A., Mithoefer, M. C., & Doblin, R. (2019). Breakthrough for trauma treatment: safety and efficacy of MDMA-assisted psychotherapy compared to paroxetine and sertraline. Frontiers in psychiatry, 10, 650.
- Horowitz, M. A., & Taylor, D. (2019). Tapering of SSRI treatment to mitigate withdrawal symptoms. The Lancet Psychiatry, 6(6), 538-546.