Initiatives to change policies and laws around psychoactive plants and fungi are moving forward in several cities and states. Organizers are harnessing various approaches to minimize penalties and advocate for wider access. Understanding the difference between legalization and decriminalization, and the implications of each, is critically important for voters, the psychedelic community, and health providers.
As the pandemic beats on, compromised mental health is affecting the lives of many in our communities. Months of isolation and collective fear over losing our health, our jobs, and our loved ones destabilizes even the most mentally fit among us. Our daily practices can help us cope with these challenges to our mental wellness.
But what will psychological and economic recovery look like when the pandemic ends? Grassroots initiatives are looking for avenues to make psychoactive plants and fungi more accessible and viable as sources for healing and well-being.
Several policy initiatives are progressing for drug reform, particularly for plant-based psychoactive substances. The call sounds across America to address prosecutions for possession of controlled substances. Furthermore, issues associated with access to regulated drug supplies also face updating. The best path forward may differ depending on the person or group you talk with. State and local initiatives are approaching policy change in various ways, either through legalization or decriminalization.
Legalization and Decriminalization: What Is the Difference?
Legalization refers to changing the status of a substance from illegal to legal. This means a person no longer faces arrest and prosecution for personal use and possession. At the federal level, psychedelic substances and cannabis currently reside on the list of Schedule I controlled substances. Changing this designation would require rescheduling by the Drug Enforcement Administration (DEA).
Clinical trials may prove that a psychedelic substance is effective for medical conditions. As a result, the FDA’s Controlled Substance staff would make a recommendation to the DEA about which category the newly approved drug should be placed in. In this case, safety data and rating for potential misuse and dependence is the basis for this reclassification.
But there’s a catch if MDMA-assisted psychotherapy or psilocybin therapy pass through clinical trials and are designated into Schedule II-V. This doesn’t mean that recreational Ecstasy or magic mushrooms would automatically be moved out of Schedule I. The DEA can differentiate between an FDA-approved medical treatment versus the same drug used in different contexts.
When a substance achieves decriminalization, this means it is the lowest priority of law enforcement. So far, Denver decriminalized psilocybin-containing mushrooms. Additionally, the three cities of Oakland, Santa Cruz, and Ann Arbor decriminalized all entheogenic plants and fungi. These successful local initiatives state that personal possession and use of these psychoactive substances would be the lowest priority for arrests and prosecution. However, state and federal laws still prohibit these substances.
Approaches for Policy Change
The grassroots efforts of Decriminalize Denver, Decriminalize Nature, and Decriminalize Santa Cruz helped these measures pass. The organizations presented evidence of the healing potential of psychedelic plants and fungi. Besides this, the groups also demonstrated their relative safety compared to other substances, and the ancient history of indigenous use in rituals and ceremonies. Local organizers seeking policy change either through ballot initiatives or through legislation should be in dialogue with native peoples. The goal is to omit peyote from resolutions. As a result, this protects diminishing peyote gardens of the Native American Church and other indigenous communities.
A different approach is underway in Oregon. The Psilocybin Mushroom Services Program Initiative (Measure 109) is on the ballot for November 2020. Measure 109 would legalize psilocybin-product manufacturing for distribution in pre-approved psilocybin service centers to individuals 21 years of age and older.
The Oregon Health Authority would provide regulations and establish the program over the next two years if the measure passes. Individuals would be able to legally buy and consume psilocybin. Consumption would occur at centers under the supervision of a licensed facilitator. Furthermore, users would not require any type of medical diagnosis to take the trip. The measure does not, however, legalize or decriminalize personal use outside of the service centers.
A separate measure (Measure 110) will be put to the vote at the same time in Oregon. This measure would incur a fine for personal possession of any controlled substance, including psilocybin. There would be a max fine of $100 or a health assessment with no more than a Class E violation.
The Psychedelic Roll-Out
Very soon many of us will have the option to take a psychedelic journey with facilitated session support. Fear of legal consequences may decrease as well. How to properly do this in the culture comes with many questions.
High on the list is how to assure subscriber safety, in addition to offering adequate preparation, information, and support. A clinic team would need medical doctors, licensed mental health professionals, and lower-credentialed individuals for supportive roles. What qualifications and training will guides or therapists require? Who will be accredited to offer training programs for licensure?
On the other hand, decriminalized cities could see the emergence of psychedelic community groups and plant medicine churches. A different set of questions arises for community-based models. But the questions continue along the same threads of risk minimization and human benefit maximization. Guidelines and credentials of trained facilitators are necessary to define standards to uphold best practices. Without oversight of medical professionals, the likelihood of adverse events increases. For the most part, trained peer providers may provide screening and safe-use guidelines. But people who are taking medications or have health conditions often need medical consultations.
Sustainability and Protections for Ancient Traditions
As demand grows, so will the questions around sourcing and sustainability of plant material or synthetic substances. Dwindling plant medicines is already a serious concern for peyote, ayahuasca, and iboga. In the end, this puts significant impact on the long-held traditions of indigenous peoples.
Conversations and regulated systems will need development and adherence, to ensure sustainability and toxin-free medicines. Moreover, there’s a need for specific protections for indigenous cultures’ ceremonial plant use, including the plants themselves. The Indigenous Peyote Conservation Initiative focuses on “empowering indigenous communities to reconnect with, regenerate, and conserve their sacred peyote medicine.” Meanwhile, the Chacruna Institute’s Council for the Protection of Sacred Plants advocates for protections of sacred plant medicines of indigenous peoples.
Decriminalization measures allow for personal growing and gifting of plants and fungi. Although, they do not give free rein to commercial growers to produce products for sale. Many speculate that magic mushrooms could follow a similar regulatory path as cannabis. However, so far the initiatives haven’t proposed mechanisms for certified growers, dispensaries, or medical cards for access.
Cost and Accessibility
Each approach comes with different costs and implications for access. If Oregon’s psilocybin services program gains voter approval, an undesirable outcomes could result. Fees associated with developing, regulating, and operating psilocybin centers could make the service costs unaffordable to many. Existing insurance coverage would not be available for psilocybin unless the FDA approves it. Furthermore, even if approved, a medical diagnosis and covering insurance provider would be required.
With legalization, non-commercial community groups or churches could potentially grow plants and fungi at small scale for gifting to their communities. Group administrations and trained peers could reduce costs compared to medically supervised individualized sessions in regulated clinical environments.
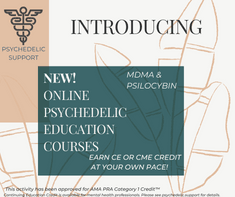
Enroll in a course, workshop, or training today.
Psychedelic Public Education
With any model there is a clear necessity for public education to promote safety and best practices. Not everyone is well suited to take a psychedelic substance. Adverse outcomes can be serious, including psychosis and even death.
Harm reduction practices should be widely available. Adults must received harm reduction education. They should be well-versed in dosing, set and setting, substance risks, and what to do when a challenging experience presents. Mechanisms are needed to keep psychedelics out of the hands of children and adolescents. Finally, educational information should be made available in age-appropriate formats.
Psychedelic.Support launched an educational program to inform health professionals and the general public about safety, effects, therapeutic modalities, and clinical trial findings. More educational content in various formats is critically needed as psychedelics reach the mainstream.