MDMA breakthrough status achieved. MDMA combined with psychotherapy is a promising treatment for PTSD and is currently under investigation in a phase 3 trial. Data from six phase 2 studies supported a Breakthrough Therapy designation by the FDA. Results are now published in Psychopharmacology.
The Multidisciplinary Association for Psychedelic Studies (MAPS) published results in Psychopharmacology [1] from six phase 2 clinical trials of MDMA-assisted psychotherapy for posttraumatic stress disorder (PTSD). PTSD is a mental disorder that can occur after a traumatic event. Symptoms include avoidance of trauma-associated places or people, negative feelings, hypervigilance and intrusive thoughts or memories. The paper describes outcomes from 103 study participants, which represents the largest sample to be published to date. These data were the basis for FDA granting a Breakthrough Therapy designation for this innovative treatment approach.
Clinical Trials Conducted
Six clinical trials were carried out from 2004-2017 at five study sites. These sites were United States (South Carolina, Colorado), Canada, and Israel. The studies enrolled people with moderate to severe chronic PTSD who had failed to adequately respond or tolerate medications and/or psychotherapies. Approximately half of patients (40-60%) do not experience significant PTSD symptom reductions from currently available medications (Zoloft and Paxil) and psychotherapies used to treat PTSD [2, 3].
For the MDMA trials, participants start treatment by undergoing three non-drug psychotherapy sessions (90 mins). Then they receive either active doses of MDMA (75-125 mg) or placebo/control doses of MDMA (0-40 mg) during 2 to 3 psychotherapy sessions that lasted for 8 hours. A male/female co-therapy team was present during all sessions, offering a supportive presence and non-directive psychotherapy. They helped create and maintain a “container” or safe space for the therapeutic experience. Because the studies were blinded, the study participants and therapy team did not know what dose they were given. Three non-drug integration sessions were conducted. During integration sessions participants worked to address and bring together, or integrate, material from the MDMA-psychotherapy sessions. Each integration session followed each MDMA session. One integration came the morning after the MDMA session, and the other two during the month proceeding the next drug-assisted session.
Results Double Down on Therapy
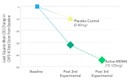
Surprisingly, the results showed that active doses of MDMA more than doubled the effect of psychotherapy alone (or with low doses of MDMA used as placebo controls). On the Clinician Administered PTSD Scale (CAPS-IV), scores dropped on average of -32.4 for the MDMA group and -10.4 for the placebo control group after two MDMA sessions. More participants in the active dose group (54.2%) did not meet criteria for PTSD compared to the control group (22.6%). PTSD symptoms significantly improved further after the third MDMA session, with an additional score reduction on average of -12.9.
Above all, doses of MDMA were well tolerated in the studies. The adverse events (undesirable effects) that occurred at greater frequency for the active MDMA group weren’t unmanageable. For instance, they included: anxiety, dizziness, jaw clenching/tight jaw, lack of appetite, and nausea. Most were mild to moderate, causing little interference with daily functioning. They resolved by the end of the session or during the week following. There were no reports or treatment discontinuation during the trial related to problematic substance use of “ecstasy” (pills that contain MDMA and other substances). As a result, this supports the low potential for developing substance use problems from taking limited doses of MDMA in a clinical setting. See the MDMA Investigator’s Brochure for all safety information from MDMA clinical trials and reviews of the scientific literature.
What Happens During MDMA-assisted Psychotherapy?
The treatment approach is described in the Manual for MDMA-assisted Psychotherapy [4]. The approach built on practices that emerged during the first wave of psychedelic explorations in therapeutic contexts in the 1950-70s. As with all psychedelics, the person’s mind set and the environment where MDMA is taken plays a key role. This is known as set and setting, which influence how a person feels and perceives the experience. For MDMA-assisted psychotherapy trials, the three preparatory sessions (90 mins each) are critically important for the participant and therapists to get to know each other and establish a trusting relationship. The therapists gain an understanding of the personal history and day-to-day struggles that the person is facing. Creating a safe and supportive environment is essential for a steady foundation for the upcoming MDMA sessions. Participants also learn practical techniques to help manage anxiety and to cope with stressful situations.
Conquering the Fear
Afterwards, participants have 2 to 3 MDMA sessions spaced a month apart. During these 8-hour psychotherapy sessions, participants can take a close inspection of traumatic memories while remaining emotionally engaged. Severe anxiety and dissociation are symptoms of PTSD that inhibit progress with talk therapy. A study participant at the Charleston, SC site described how different MDMA-assisted psychotherapy was compared to other therapies by saying,
“I had a lot of defenses going up into the therapies that I had previous to the MDMA, and it made accomplishing any substantial breakthroughs in what I was going through pretty impossible. So with the MDMA, it broke this hard, outer shell that was up that kept me from being able to connect with the therapies I was going through [5].”
Comfort to Overcome Fear
MDMA can reduce fear and resistance to explore painful memories while allowing the person to more fully experience difficult feelings, such a pain, shame, and grief, without becoming overwhelmed or numbed out. The environment and interactions with the therapists support the therapeutic process with MDMA, as described by a person with PTSD who underwent treatment:
“I think that the MDMA gave me the ability to feel as though I was capable and safe of tackling the issues. Whereas before I feared those thoughts and I tried to avoid them at all times, and avoid things that reminded me of those thoughts, I think it allowed me to feel safe in my space. Of being able to fight it. I felt like I had the ability and tools, whereas before I was unarmed, unarmored, and had no support. And this type of environment, with (the therapists), the catalyst drug, and everything else, it felt as though I had backup. Now it was safe and I had my tools and weapons to be able to tackle the obstacles that I never had before [5].”
Activates Deep Healing
The combination of the drug plus therapy can facilitate a deep a healing and release of entangled emotions that may have been otherwise inaccessible. Participants describe a speeding up of a process to get to the root of where their PTSD symptoms stem.
“I just think it would have been several more years of painful maybe terrible therapy that went nowhere. I feel like this therapy really helped me get past the tears and get right to the problem and several other problems I didn’t know were related to the feeling,” said a MAPS’ trial participant [5].
It’s thought the combination of the MDMA, the therapists, and the supportive setting create optimal conditions for a person to heal their psychological wounds. The therapists offer encouragement and an empathetic presence, supporting whatever is coming up for the person without directing the therapeutic process.
A New Future by Illuminating the Past
Like a prism, MDMA sheds new light on a person’s past, illuminating fractured parts of the self that can be stitched back together to instill a sense of wholeness. It can be a transformative treatment that reminds a person that the present is the time and place to live, and past hardships can be reframed through a lens of compassion and empathy.
One study participant described this as, “It was really that first MDMA session that we had, where I had that, I consider it a breakthrough, where I was able to clearly see that I had a big disconnect in compassion for myself [5].”
Novel Insights Arise
Novel insights and shifts of perspectives often arise, allowing for corrective experiences through the process of forgiveness, acceptance, and a sense of wellbeing. The therapists and participant continue therapeutically process during the 3 integrative sessions that follow each MDMA session.
“I’m definitely better, but I’ve got to continue on. This isn’t something that you take a pill or push a button and say, “I’m well.” (It is something I) will be working on for a long time. (But) I have definitely moved light years ahead in a short period of time [5].”
The participants said as their PTSD symptoms decreased, they were more fully able to engage in life and relationships in ways that were not possible before undergoing MDMA-assisted psychotherapy. At the long-term follow-up visit 12 months after completing the treatment, more people did not meet PTSD criteria (68%) than at study exit, defined as the last time their PTSD symptoms were measured (1 to 2 months after their last MDMA session).
Brains on MDMA Breakthrough– Possible Mechanisms for Therapeutic Effects
Because MDMA targets several neurotransmitters (serotonin, norepinephrine, dopamine) and increases hormone levels (oxytocin, cortisol, vasopressin, prolactin), many neurobiological mechanisms likely underlie the therapeutic effects. Going beyond a biological explanation, psychological and psycho-spiritual aspects of MDMA-assisted psychotherapy are paramount for understanding the full spectrum of therapeutic effects.
In human brain imaging, MDMA decreases activity in the amygdala in response to negative emotional stimuli (angry facial expressions) [6], which may partially explain why people with PTSD can more readily revisit traumatic memories while staying emotional engaged. Another imaging study showed that MDMA causes more crosstalk between the amygdala and hippocampus – hubs for memory and emotional processing [7]. When trauma memories are recalled during MDMA sessions, additional information may be incorporated into the memory traces, allowing for them to be filed back in the brain in a way that signifies the threats of the past are no longer part of the present moment. This is referred to as memory reconsolidation and could be one way that MDMA is working during talk therapy [8].
Animal Studies
Translation of findings from animal models to humans is not without limitations, but these studies can give us a better idea of how a drug is acting in the brain. MDMA has been widely investigated in rodents to understand the effects of “Ecstasy”. But most rodent experiments tested extremely high, repeated doses of MDMA that were not close to what humans consume. The dose and the context are interplaying factors, each significantly contributing to subjective experience.
Now researchers are using doses closer in the range of those used in human clinical trial in experiments designed to mimic PTSD or further characterize MDMA. The goal is to understand what is happening in the brain to produce such dramatic improvements in PTSD symptoms, and to understand possible ways to optimize this treatment.
MDMA Rewards Social Activity
A recent publication in Nature found that MDMA makes social activity more rewarding to mice, similar to how mice respond when they are younger. The effects on social behaviors lasted for up to 2 weeks after MDMA. The experiments found this response depended on increased oxytocin release from MDMA-stimulated serotonin elevations in the nucleus accumbens, a region of the brain important for signaling reward [9]. Prosocial effects after MDMA have also been shown in octopuses, zebra fish, and rodents [10, 11]. Social behavior between unfamiliar mice also increases with successive doses of MDMA that are moderately higher than those given to humans. These findings suggest that MDMA enhances social reward learning. As a result, this could explain the observed increased therapeutic alliance between the co-therapy team and participants undergoing MDMA-assisted psychotherapy.
Fear Extinction
Other studies in rodents have posited that the reductions in PTSD symptoms are due to fear extinction and memory reconsolidation. Mice trained to associate a foot shock with an auditory tone were more quickly able to forget that the tone signified a negative stimulus when given MDMA. The effect was dependent on increased bran derived neurotrophic factor (BDNF), a signaling molecule involved with neuroplasticity, in the amygdala. This finding suggests new adaptations in the brain region that fires up in response to fear [12].
A different study in rats showed that MDMA blocked the reconsolidation of fear memories but failed to detect enhancement of fear extinction which relies on different pathways in the brain [13]. Discrepancy in findings between these two studies could be from the different species used (rats vs. mice) or from variations in experimental designs. A study in humans is currently underway at Emory University investigating MDMA and fear extinction with a startle response model.
As we learn more about how MDMA works in the brain when administered in specific contexts, other types of approaches and therapeutic modalities may find that MDMA can bolster treatment outcomes. Planning to investigate this question with new research trials is underway. Moreover researchers want to see if MDMA-assisted psychotherapy could be useful for other psychiatric indications. For example, future studies may address eating disorders, substance use disorders, and other anxiety-related conditions.
Current Affairs for MDMA Breakthrough Research
In August 2017, the FDA granted Breakthrough Therapy designation for MDMA-assisted psychotherapy for treating PTSD after reviewing the results from the six phase 2 trials. Comparison of findings from MDMA trials to results that led to the approval of sertraline (Zoloft) and paroxetine (Paxil) for PTSD, suggest that MDMA-assisted psychotherapy could have substantial improvement and lower overall risk than existing medications used to treat PTSD. Since MDMA is given three times in a clinic, it has fewer side effects and lower risks than take home medications that are taken daily for extended periods.
At the present time MDMA-assisted psychotherapy is in the final round of testing for two phase 3 trials. These studies will enroll approximately 200-300 participants with severe PTSD at 15 study sites in the USA, Canada, and Israel. If results replicate the phase 2 MDMA breakthrough trials, then MDMA could be approved for use in therapy for treating PTSD by 2021.
Clinicaltrails.gov Records for studies included the Psychopharmacology publication [1]:NCT00090064, NCT00353938, NCT01958593, NCT01211405, NCT01689740, NCT01793610
References
- Mithoefer, M.C., Feduccia, A.A., Jerome, L., Mithoefer, A., Wagner, M., Walsh, Z., Hamilton, S., Yazar-Klosinski, B., Emerson, A., and Doblin, R. (2019). MDMA-assisted psychotherapy for treatment of PTSD: Study design and rationale for Phase 3 trials based on pooled analysis of six Phase 2 randomized controlled trials. Psychopharmacology.
- Bradley, R., Greene, J., Russ, E., Dutra, L., & Westen, D. (2005). A multidimensional meta-analysis of psychotherapy for PTSD. American journal of Psychiatry, 162(2), 214-227.
- Brady, K., Pearlstein, T., Asnis, G. M., Baker, D., Rothbaum, B., Sikes, C. R., & Farfel, G. M. (2000). Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. Jama, 283(14), 1837-1844.
- Mithoefer, M.et al. (2017). A Manual for MDMA-Assisted Psychotherapy in the Treatment of Posttraumatic Stress Disorder. MAPS, Version 8. http://www.maps.org/research/mdma/mdma-research-timeline/4887-a-manual-for-mdma-assisted-psychotherapy-in-the-treatment-of-ptsd.
- Barone, W., Beck, J., Mitsunaga-Whitten, M., & Perl, P. (2019). Perceived Benefits of MDMA-Assisted Psychotherapy beyond Symptom Reduction: Qualitative Follow-Up Study of a Clinical Trial for Individuals with Treatment-Resistant PTSD. Journal of psychoactive drugs, 1-10.
- Bedi, G., Phan, K. L., Angstadt, M., & De Wit, H. (2009). Effects of MDMA on sociability and neural response to social threat and social reward. Psychopharmacology, 207(1), 73.
- Carhart-Harris, R. L., Murphy, K., Leech, R., Erritzoe, D., Wall, M. B., Ferguson, B., … & Tanner, M. (2015). The effects of acutely administered 3, 4-methylenedioxymethamphetamine on spontaneous brain function in healthy volunteers measured with arterial spin labeling and blood oxygen level–dependent resting state functional connectivity. Biological psychiatry, 78(8), 554-562.
- Feduccia, A. A., & Mithoefer, M. C. (2018). MDMA-assisted psychotherapy for PTSD: are memory reconsolidation and fear extinction underlying mechanisms? Progress in neuro-psychopharmacology and biological psychiatry, 84, 221-228.
- Nardou, R., Lewis, E. M., Rothhaas, R., Xu, R., Yang, A., Boyden, E., & Dölen, G. (2019). Oxytocin-dependent reopening of a social reward learning critical period with MDMA. Nature, 1.
- Stewart, A., Riehl, R., Wong, K., Green, J., Cosgrove, J., Vollmer, K., … & Gaikwad, S. (2011). Behavioral effects of MDMA (“Ecstasy”) on adult zebrafish. Behavioural pharmacology, 22(3), 275.
- Edsinger, E., & Dölen, G. (2018). A conserved role for serotonergic neurotransmission in mediating social behavior in octopus. Current Biology, 28(19), 3136-3142.
- Young, M. B., Andero, R., Ressler, K. J., & Howell, L. L. (2015). 3, 4-Methylenedioxymethamphetamine facilitates fear extinction learning. Translational psychiatry, 5(9), e634.
- Hake, H. S., Davis, J. K., Wood, R. R., Tanner, M. K., Loetz, E. C., Sanchez, A., … & Greenwood, B. N. (2019). 3, 4-methylenedioxymethamphetamine (MDMA) impairs the extinction and reconsolidation of fear memory in rats. Physiology & behavior, 199, 343-350.