Depression is one of the most common mental health conditions in the world; it is estimated that one in six people will be affected by depression at some point in their life. Anyone can experience depression, even those who seem to live happy and healthy lives are susceptible to this medical illness.
It’s important to remember that there is no single cause for depression and that sometimes it happens to people without a known cause at all. In addition, everyone experiences depression differently with different symptoms, behaviors, reactions and responses.
Depression is not always preventable; researchers agree that there are multiple factors that can contribute to a person experiencing depression such as genetics, physical health issues, brain chemistry and lifestyle causes.
Let’s take a look at some of the most common causes of depression.
Brain Chemistry Causes Depression
A potential cause of depression is due to brain chemistry; specifically, those with depression may have a chemical imbalance in areas of their brain that are responsible for regulating behavior, mood, thoughts, appetite, and sleep.
The specific chemical substances involved are called neurotransmitters, including norepinephrine, dopamine and serotonin. Neurotransmitters allow different parts of the brain to communicate by sending messages to each other.
It is suggested that if there is an imbalance of these neurotransmitters, such as an excess or an inadequate amount, it can result in or contribute to symptoms of depression.
Therefore, many medications that treat depression were designed to balance brain chemistry. Some of these include tricyclic antidepressants (TCAs), monoamine oxidase inhibitors (MAOIs), selective serotonin reuptake inhibitors (SSRIs), and serotonin-norepinephrine reuptake inhibitors (SNRIs).
Although this is one of the most well-known causes and medications were created based on it, it doesn’t provide a full understanding of all the different factors that can contribute to depression. Read on to learn more about other potential causes of depression.
Brain Structure Causes Depression
There are specific parts of the brain that manage mood; therefore, researchers suggest that the way the brain is structured can be a potential cause of depression.
A study looked at 24 women with a history of major depression and compared them with 24 case-matched controls. Both groups underwent magnetic resonance imaging (MRI) scanning to measure the size of their hippocampus. The results showed that the women with depression had significantly smaller hippocampal volumes bilaterally and smaller amygdala core nuclei volumes than the control group. In addition, an increased frequency of depression was associated with a smaller hippocampus. The study suggested that stress may explain volume loss as it can inhibit the growth of new neurons in the hippocampus.
The amygdala is a part of the brain that plays a role in intense emotions such as fear, anger, sadness, sexual arousal and pleasure. In those who are depressed, the amygdala is enlarged and has increased activity compared to those who are not depressed.
Hormone Levels Causes Depression
Hormonal factors may play a role in depression. For instance, women are more likely than men to experience depression with a prevalence of 10.5% and 6.2%, respectively. Specifically, it is during a woman’s reproductive years when depression occurs most often.
The changing levels of hormones, including progesterone and estrogen, that occur during a woman’s menstrual cycle, childbirth, postpartum and perimenopause, are thought to contribute to depression. After menopause, the incidence of depression in women decreases.
Some women experience postpartum depression after giving birth. The sudden changes in hormone levels, additional responsibility for a child, lack of sleep, and adjusting to a new routine can all contribute to their risk for depression.
Childhood Trauma Causes Depression
If someone experienced trauma during their childhood, it can affect how their brain reacts to stress, threats and fears. Childhood trauma can extend into adulthood and manifest as symptoms of depression.
Some examples of childhood trauma include sexual, physical or verbal abuse, domestic violence, life-threatening illness, unstable environment, neglect and death of a loved one.
Medical Conditions
There is a strong connection between the mind and body. For instance, if you’re struggling with a physical illness, it can negatively impact your mental health and vice versa.
Certain medical conditions such as chronic illnesses or pain, can increase the risk of someone experiencing depression. Some of these conditions include diabetes, autoimmune diseases, including systemic lupus erythematosus, rheumatoid arthritis and psoriasis, Parkinson’s disease, insomnia, hypothyroidism, multiple sclerosis, cancer, stroke, obesity and heart disease.
In addition, some medications that are used to treat chronic illnesses can increase the likelihood of depression.
Follow your Curiosity
Sign up to receive our free psychedelic courses, 45 page eBook, and special offers delivered to your inbox.Genetics and Family History
A person is more vulnerable to depression if someone in their family had it or another type of mood disorder. However, someone without a family history of depression can also be at risk for depression.
An article reviewed family, twin and adoption studies as well as genome-wide association and linkage studies to understand the role of genetics in the development of depression. It explained that there are genetic components that cause depression; however, there isn’t a single genetic variation that increases the risk substantially. It concluded that the risk for depression is more likely the result of a combination of genetic and environmental factors.
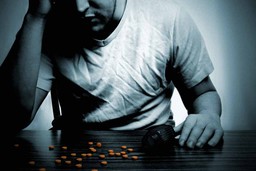
Substance Misuse
Some people cope with stress and health issues by drinking alcohol or taking drugs. However, this can contribute to and worsen symptoms of depression.
Those who have a substance use disorder are more likely to experience depression. Alcohol has been shown to disrupt the brain’s chemical balance. Long-term excessive drinking can also lead to medical conditions such as cancer, heart disease, high blood pressure, liver disease and stroke.
Seasonal Changes
Seasonal Affective Disorder (SAD) is a type of depression that occurs when the seasons change. Specifically, people who have SAD tend to feel depressed when daylight hours become shorter.
Studies show that people with SAD have a lower level of serotonin which can affect how they regulate their mood and interfere with the quality of their sleep. Season changes can increase the level of melatonin in the body, causing someone to feel more sleepy than usual.
An insufficient diet of vitamin D and reduced exposure to sunlight during the winter time can also contribute to SAD and be part of what causes depression. When the body doesn’t have enough vitamin D, it can decrease the production of serotonin.
Other Causes
Other factors that can also contribute to depression include relationship problems, a diet lacking essential nutrients, loneliness, social isolation, aging, family issues, the death of a loved one, medications, and major stressful life events such as job loss, divorce, and retirement.
If you, a friend or a loved one is struggling with depression, it’s important to seek help from a healthcare professional to explore treatment options. For most people, depression is treatable and they are able to manage their symptoms and live fulfilling and happy lives.
References
- National Institute of Mental Health. Major depression.
- Weissman MM, Berry OO, Warner V. A 30-year study of 3 generations at high risk and low risk for depression. JAMA Psychiatry. 2016;73(9):970–977.
- Nutt DJ. Relationship of neurotransmitters to the symptoms of major depressive disorder. J Clin Psychiatry. 2008;69 Suppl E1:4–7.
- Sheline YI, Sanghavi M, Mintun MA, Gado MH. Depression duration but not age predicts hippocampal volume loss in medically healthy women with recurrent major depression. J Neurosci. 1999;19(12):5034–5043.
- Lohoff FW. Overview of the genetics of major depressive disorder. Curr Psychiatry Rep. 2010;12(6):539–546.
- Soares CN, Zitek B. Reproductive hormone sensitivity and risk for depression across the female life cycle: A continuum of vulnerability? J Psychiatry Neurosci. 2008;33(4):331–343.
- Postpartum depression. https://www.apa.org.
- National Institute of Mental Health. Chronic illness & mental health.
- Ng E, Browne CJ, Samsom JN, Wong AHC. Depression and substance use comorbidity: What we have learned from animal studies. Am J Drug Alcohol Abuse. 2017;43(4):456–474.
- National Institute of Mental Health (NIMH). Seasonal affective disorder.